Today, the total number of Americans with mental illnesses sums to around 44 million; that’s nearly one in five Americans suffering from mental health problems (1). These unfortunate statistics bring into question the topic of diagnosis. How are mental health disorders detected, categorized, and treated? This article will seek to explore these topics. Specifically the history, current applications, criticisms, and implications of the various frameworks that are currently being used to identify, study, and treat mental health conditions.
The Diagnostic and Statistical Manual of Mental Disorders (DSM)
The Diagnostic and Statistical Manual of Mental Disorders (DSM) is a handbook that was originally published in 1952 by the American Psychiatric Association (APA). The DSM was the first official manual of mental disorders to focus on clinical use. The DSM has since been considered the “gold standard” for diagnosing mental health disorders. Over the years, the DSM has undergone several revisions to update and reorganize its diagnostic criteria. Currently, the DSM is in its fifth edition (DSM-V) and has served as a revolutionary manual for understanding, classifying, studying, and standardizing mental health disorders in America and around the world.
Since its publication, the DSM has been subject to strong criticisms. Scientists and mental healthcare workers have called into question the DSM’s symptomatic categorization of mental health disorders. One of the prominent challenges the DSM has faced is that a multitude of diverse behaviors that can arise from a single disorder, and identifying which symptom belongs to which disorder can be tricky. In addition, there is often significant individual variation of symptoms among people suffering from the same disorder. This problem is known as phenotypic heterogeneity. To illustrate the problem of phenotypic heterogeneity, consider a concrete example: in the fifth edition of the DSM, there are “256 different sign/symptom combinations [that] are compatible with a diagnosis of borderline personality disorder. As an even more extreme example, in DSM-V, there are 636,120 ways to meet diagnostic criteria for PTSD” (2). Due to the incredibly extensive signs/symptoms that can arise from a single disorder, it is understandable how the DSM can lend itself to extreme confusion when a psychiatrist needs to diagnose a patient. This confusion can and has led to high rates of misdiagnosis. Since the DSM relies heavily on symptom-based self-reports from the patient, there exists a potential for the patient to misinform, and also for patients to lie to their doctor about what they are experiencing. This was backed by a 2018 study that found 81% of patients will avoid disclosing at least one type of information to their doctor (3).
The criticism that the DSM has faced does not stop at phenotypic heterogeneity. Equally concerning are the issues of comorbidities and shared pathophysiologies. These topics have plagued the efficacy of the DSM for years. Comorbidities refer to two or more conditions present in one individual and shared pathophysiologies refer to a similar symptom across multiple conditions. A 2016 paper pointed out that, “In the eyes of many authors, the presence of rampant comorbidity is a red flag that the DSM system is not drawing the correct diagnostic borders” (2). Criticisms like this among many others have called into question if the DSM’s symptomatic categorization method of diagnosis is reliable.
A few weeks before the APA’s release of the fifth edition of the DSM, former National Institute of Mental Health (NIMH) Director Thomas Insel announced that the NIMH “will be re-orienting its research away from DSM categories” (4). Instead, the NIMH would reallocate funding towards developing a better system for understanding mental health. This was a major hindrance to the DSM since researchers using it would need to change their approach to studying mental health disorders if they wished to receive funding for their projects. This shift has led to an overall decreased enthusiasm for the DSM and increased enthusiasm for alternative biologically driven methods of studying mental health.
Given the aforementioned shortcomings, an up-to-date view of the DSM leads to the understanding that there is a tendency to oversimplify and over-diagnose mental health disorders. This is done by standardizing and compartmentalizing aspects of behavior without enough emphasis on individual variation. The need for a new system of understanding and advancing mental health was met in 2009 when the NIMH announced the arrival of a new project.
The Research Domain Criteria (RDoC) Project
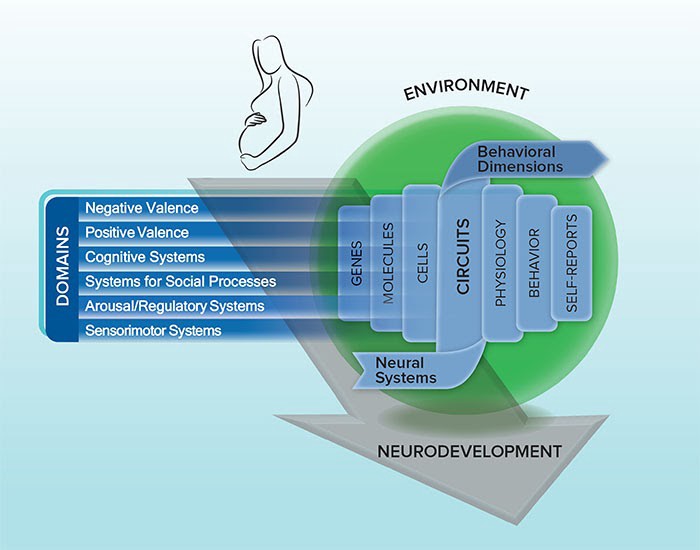
In 2009, under the direction of Thomas Insel, the NIMH launched a new initiative: The Research Domain Criteria (RDoC) project. Unlike the DSM, the RDoC project is not a diagnostic tool, rather it is a research framework for investigating mental health with the goal of providing information about the basic biological and cognitive processes that lead to mental health illness (5). The intention behind the NIMH’s launch of the RDoC project was to create a new approach to understanding mental health from different perspectives. One of the key ideas behind the RDoC initiative was to reframe our thinking about “mental disorders” and begin to understand them as “brain disorders”. This shift in thinking requires a biologically driven systematic approach for understanding mental health. This means researchers using the RDoC framework might utilize different kinds of technologies to gather information about biological functions. An example of this is neuroimaging modalities such as MRI/fMRI, PET, EEG, and DTI. Additionally, researchers might gather other kinds of biological metrics such as heart rate variability (HRV), sleep pattern information, and hormonal measurements in the body. However, it doesn’t stop there as new technologies are constantly emerging which might help to better inform researchers about mental health and brain disorders. This biology-driven approach is one of the strengths of the RDoC framework.
The RDoC was created out of a widespread recognition that studying mental health through traditional diagnostic criteria such as the method employed by the DSM, has “not significantly advanced our understanding of mental illnesses for some time” (6). It is fair to say that the RDoC was created in part as a response to the inadequacies of the DSM and strives to correct issues of phenotypic heterogeneity, comorbidities, and shared pathophysiologies by incorporating biological approaches to identifying brain disorders.
The RDoC framework expands upon the DSM’s subjective symptom-based diagnostic categorization by incorporating six unique domains: Positive and Negative Valence, Cognitive Systems, Systems for Social Processes, Arousal/Regulatory Systems, and Sensorimotor Systems. Furthermore, the RDoC looks across multiple environments including Genes, Molecules, Cells, Circuits, Physiology, Behavior, and Self Reports. This “Diagnostic Matrix” is an exhaustive approach to understanding mental health disorders and has the potential to resolve many of the issues that traditional diagnostic methods like the DSM have faced.
Earlier this year, the current director of the NIMH, Joshua Gorden wrote in a blog post, “as RDoC passes its 10th anniversary, we seek to increase the focus on flexibility, testing and refining these constructs and exploring their clinical utility” (8). It is clear that the future of the RDoC is bright and holds massive potential to reshape the way that scientists and psychiatrists alike understand and diagnose brain disorders. With that said, the RDoC framework is not yet ready to be accepted for clinical use. One of the challenges presented is the price of obtaining biological metrics. Some metrics cost less than others. For example, it might cost $200 or less to track sleep patterns but the average price for an MRI brain scan is around $2,600 or more (9). This financial issue brings into question if the RDoC could ever fully replace a simpler and less expensive (but more generalized) method of diagnoses like the DSM. The fact remains that the RDoC framework has encouraged significant advances over the past decade. The NIMH is currently exploring the clinical utility of the RDoC framework as the current state of mental health diagnosis shifts towards a more biologically driven approach.
The Brain and Precision Medicine
The brain is an unimaginably complex organ with 100 billion neurons and 100 trillion synaptic connections. Scientists are just beginning to figure out how to understand the connections in the human brain. Although there is not a complete understanding of the brain quite yet, experts can identify when brain circuits are wired in problematic ways. Take for example a disorder like Schizophrenia; there are specific predictable patterns in the neural circuitry that indicate risk for Schizophrenia onset. Those predictable patterns would be considered risk factors for a person developing Schizophrenia. In other words, scientists are able to identify people who might be at greater risk for developing a disorder just based on their brain imaging data or other biological metrics. This means that with the current technologies available, scientists can detect brain disorders before behavioral symptoms arise. This is an incredibly important point because when it comes to brain disorders, behavioral symptoms are the LAST thing to appear. Changes in gene expression, molecules, cells, and circuits all arise before any behavioral changes. This has massive implications for the field of mental health because patients will be able to receive treatment for an illness PRIOR to that illness arising as a problematic behavior (7). This understanding brings us to the topic of precision medicine which can be described as the ability to identify precisely what is wrong and to create a uniquely appropriate response for each patient. Precision medicine and translational neuroscience are closely tied together since the goal of translational neuroscience is to take the knowledge gained through scientific observation and turn that knowledge into practical interventions and applications for treating human disorders and illnesses.
Conclusion
In many ways, the DSM has served its purpose well. It has revolutionized and standardized psychiatric disorder classification by identifying the core components of mental health conditions. It has also helped to advance scientific investigation in psychopathology. Due to its history and widespread use, the DSM has been considered the “gold standard” for researchers and psychiatrists alike for many years. However, due to intense criticisms, a lack of specificity, issues with polygenetic heterogeneity, comorbidity, and shared pathophysiologies the focus on the DSM is declining. A widespread desire for greater advances in the field of psychiatric medicine and the desire for a more precise system of understanding mental health has paved the way for the arrival of the RDoC.
As technology continues to advance so have our methods of using technology to identify and study mental health and psychopathology. The introduction of the RDoC symbolizes advancement in the direction that the study of mental health is headed. “The RDoC initiative developed out of an explicit desire to support translational neuroscience in mental health research” (2). Although the RDoC is currently a research framework and not a clinical tool, it has been shifting attention away from the DSM and onto a more dynamic, systems-based, biologically driven approach to understanding mental health.
Scientific investigation into mental health disorders has given rise to the understanding that individual variation is so great that a precision medicine approach is needed in psychiatry. Furthermore, a precision medicine approach is the best path for patients as it will ensure specific and individualized care. The RDoC also has the potential to improve the quality of life for countless amounts of people by identifying the early onset of disorders in high-risk individuals. With that said, the costs of utilizing the RDoC framework for diagnosing patients is not yet fully understood.
Although imperfect, the excitement for RDoC ushering in a new diagnostic approach to mental health has never been greater. Will the DSM remain an integral part of mental health diagnosis or will it be entirely replaced with a more biologically-driven, systematic approach such as the RDoC? Only time will tell. We can say for certain that the value the RDoC has provided to mental health research is overwhelmingly positive. As our understanding of mental health continues to evolve we just might begin to see biological markers become the new norm in mental health diagnosis.